Pakistan’s melting glaciers are ‘erupting’ and worsening floods
The changing climate has had a profound effect on the natural environment, particularly in regions that are already vulnerable to extreme weather events. In Pakistan, the combination of rapidly melting glaciers in the northern mountainous regions and increasingly intense monsoon rains has brought forth a growing public health concern. This dual environmental challenge has not only led to widespread flooding and displacement but has also created ideal conditions for the spread of waterborne diseases. As glaciers in areas like Gilgit-Baltistan continue to retreat at an alarming rate, the glacial lakes they leave behind become increasingly unstable. When these lakes burst, they send massive volumes of water downstream, compounding the effects of seasonal monsoon rainfall. The resulting floods overwhelm communities and local infrastructure, setting the stage for a serious health crisis.

In many affected regions, particularly rural districts along river basins, families have found themselves suddenly surrounded by contaminated water. This water seeps into wells, irrigation systems, and drinking supplies, creating a breeding ground for bacteria, viruses, and parasites. Communities that depend on river water for daily needs often have no alternative sources during flood events. Without proper sanitation, safe drinking water, or adequate health services, residents begin to fall ill from diseases such as cholera, dysentery, hepatitis, and various forms of gastroenteritis. Even simple tasks like washing hands or preparing food become dangerous when clean water is unavailable. The problem intensifies when floodwaters recede slowly, leaving behind stagnant pools where mosquitoes and other vectors thrive, further compounding health risks

Pakistan’s melting glaciers are ‘erupting’ and worsening floods
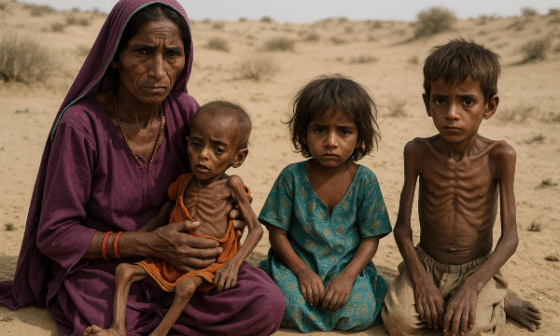
In such scenarios, it is often the most vulnerable populations who suffer the most. Pregnant women, young children, and the elderly are especially at risk from dehydration, malnutrition, and untreated infections. In recent flood emergencies, local clinics and field hospitals have reported a significant increase in cases of high fever, vomiting, diarrhoea, and skin infections. One doctor working in a mobile health unit described treating mothers who carried ill children for hours just to reach a safe place. In temporary shelters, where people are crowded and hygiene conditions are poor, illnesses spread quickly from one person to another. The lack of clean latrines, soap, and water purification tools makes it almost impossible to prevent new outbreaks from occurring in these environments.

Pakistan’s melting glaciers are ‘erupting’ and worsening floods
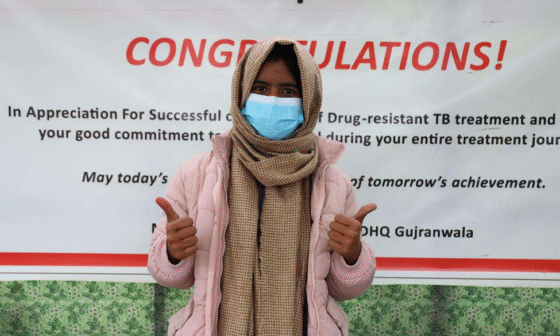
Health workers across the country have responded with dedication and resilience, setting up temporary clinics and conducting emergency vaccination campaigns. Aid agencies and non-governmental organizations have played an important role in delivering hygiene kits, oral rehydration salts, mosquito nets, and clean drinking water. However, these efforts are often hindered by damaged roads, communication breakdowns, and limited supplies. In areas that are difficult to access, many families wait days before receiving help. While the response has saved countless lives, it also highlights the fragility of the current health infrastructure when confronted with climate-driven emergencies. Some clinics have been forced to operate without electricity or clean water, while others struggle to cope with the influx of patients.

Personal accounts from those directly affected by the crisis reveal the emotional and psychological toll of these events. In southern Pakistan, one woman recounted how she lost both her home and her livestock during a flood and was later hospitalized for a waterborne infection after drinking from a contaminated stream. Another man described how floodwaters reached the roof of his house and forced his entire family to live on a nearby roadside for several weeks. These real-life experiences underline that beyond the statistics and headlines, there are human beings facing uncertainty, trauma, and long-term health consequences. Their stories are a sobering reminder of the need for long-term planning, investment, and climate resilience strategies that prioritize both environmental safety and public health.
In response to this ongoing crisis, there is an urgent need for a multi-layered approach that addresses both the environmental and health dimensions of climate change. Early warning systems for glacial lake outbursts and improved forecasting for monsoon rains can help communities prepare in advance. Investment in clean water infrastructure, flood-resilient sanitation systems, and permanent health facilities is essential. Public awareness campaigns that promote hygiene practices and disease prevention must also be expanded, particularly in high-risk regions. Furthermore, collaboration between government agencies, local communities, and international organizations can build the capacity needed to respond more effectively in the future. Only by viewing health and climate as interconnected challenges can Pakistan hope to reduce the risks of disease and protect the well-being of its people.
References
The Guardian. (2025). Accelerated Glacial Melt and Monsoon Rains Trigger Deadly Floods in Pakistan. Retrieved from theguardian.com
Dawn News. (2025). Experts Warn of Surge in Waterborne and Vector-borne Diseases After Recent Floods. Retrieved from dawn.com
Red Cross UK. (2024). Risk of Waterborne Disease After Pakistan Floods. Retrieved from redcross.org.uk
Al Jazeera. (2022). How Floods are Reshaping Pakistan’s Public Health System. Retrieved from aljazeera.com UNICEF. (2023). Children in Flood-affected Areas at Risk of Disease and Malnutrition. Retrieved from unicef.org