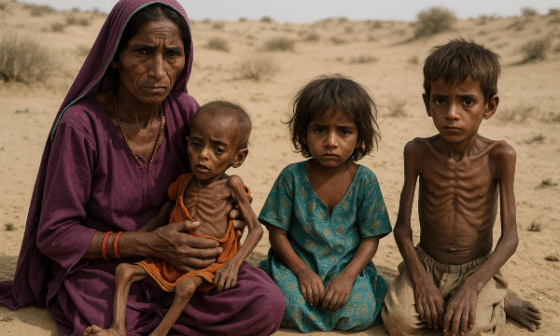
Maternal health remains one of the most pressing healthcare concerns in remote regions of Pakistan, where access to quality medical facilities is extremely limited. Every year, thousands of women face preventable complications during pregnancy and childbirth simply because they lack skilled medical care. According to national health statistics, maternal mortality rates are significantly higher in rural and mountainous areas compared to urban centers like Karachi or Lahore. Poor infrastructure, cultural taboos, lack of awareness, and a severe shortage of trained healthcare professionals exacerbate the problem. Women in remote communities often rely on untrained birth attendants or traditional midwives, which increases the risk of infections, excessive bleeding, obstructed labor, and even death. Addressing these challenges is critical not only for saving lives but also for breaking the cycle of poverty and poor health that affects entire families.

Addressing ‘Obstetric Violence’ in Africa | Human Rights Watch
In the rugged valleys of Gilgit-Baltistan, 23-year-old Fatima went into labor late one winter night. With heavy snow blocking the roads and no nearby health facility, her family had no choice but to call a traditional birth attendant from the village. The delivery became complicated when the baby got stuck in the birth canal, but the midwife lacked the skills and tools to handle the emergency. By the time Fatima was transported to the nearest hospital—three hours away—she had lost a significant amount of blood. Sadly, Fatima did not survive, leaving behind a newborn child and a grieving family. Her story is heartbreakingly common in many rural pockets of Pakistan, where geography, poverty, and lack of trained medical help turn childbirth into a life-threatening event.
One of the core issues behind poor maternal health outcomes is the shortage of skilled birth attendants (SBAs). In many rural areas, women prefer to give birth at home due to cultural beliefs or the fear of being judged in hospitals. Even when they wish to seek medical care, the nearest facility may be miles away with no reliable transport. Furthermore, poverty prevents families from affording hospital deliveries, pushing them toward cheaper but unsafe alternatives. Many rural health centers remain understaffed, and when SBAs are available, they often lack essential medical equipment or proper supervision. The shortage of female healthcare providers is another barrier, as cultural norms in conservative areas discourage women from being treated by male doctors. All these factors collectively increase the risk of maternal mortality and morbidity.

Investing in Birth Attendants Reduces Maternal Mortality and Improves Overall Care
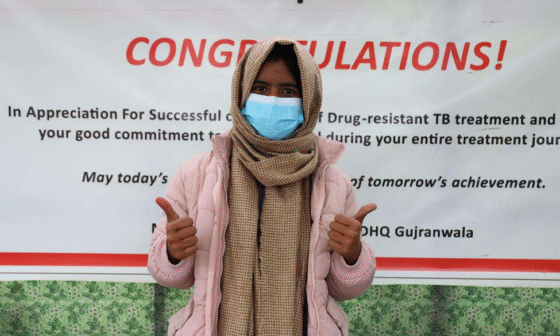
The solution lies in strengthening the network of skilled birth attendants and integrating them into rural healthcare systems. SBAs are trained professionals—midwives, nurses, or doctors—who are equipped to handle normal deliveries safely and detect complications early. Expanding community midwifery programs can ensure that trained personnel are present in every village, reducing delays in emergency care. Programs that train local women as midwives have proven effective in increasing trust and acceptance within communities. Additionally, mobile health units can bring services closer to remote villages, while telemedicine platforms can connect rural SBAs to urban specialists for real-time guidance. Awareness campaigns in local languages should educate families on the importance of safe deliveries and the dangers of relying solely on traditional methods.

Midwives Lead the Way: The 5th Global Midwifery Symposium | New Security Beat
Government policies and NGO interventions play a critical role in improving maternal health outcomes. Strengthening Lady Health Worker (LHW) programs, building maternity waiting homes near district hospitals, and subsidizing the cost of skilled delivery services are essential steps. Collaborations between public and private sectors can ensure consistent funding and training for SBAs. In addition, transport initiatives like community-run ambulances can significantly reduce delays in reaching medical facilities. Lessons can be drawn from successful maternal health projects in countries like Bangladesh and Nepal, where community midwives have drastically reduced maternal deaths in rural areas. If implemented strategically, such models can be adapted to Pakistan’s unique cultural and geographic context.

5 drivers of women and children’s health in under-served communities | World Economic Forum
Maternal health is a fundamental human right, and no woman should lose her life while bringing another into the world. Fatima’s story reflects the harsh reality faced by countless women in Pakistan’s remote regions, but it also highlights the power of timely intervention. With investment in skilled birth attendants, improved infrastructure, and widespread community education, these tragedies can be prevented. Bridging the gap between rural communities and essential maternal healthcare is not just a medical necessity but a moral responsibility. By prioritizing maternal health, Pakistan can build stronger families, healthier generations, and more resilient rural societies.
References
Human Rights Watch (2023). “Maternal Health as a Human Rights Issue in Developing Countries.”
World Health Organization (2023). “Skilled Birth Attendance: Key to Reducing Maternal Mortality.”
National Institute of Population Studies (2022). “Pakistan Maternal Mortality Survey.”
UNICEF Pakistan (2023). “Maternal Health Challenges in Rural and Remote Communities.”
Journal of Global Health (2022). “Community Midwifery Programs in South Asia.”
The Lancet Public Health (2023). “Bridging Maternal Health Gaps Through Skilled Care.”
Aga Khan University Research (2022). “Training Rural Women as Skilled Birth Attendants in Gilgit-Baltistan.”
Dawn News (2023). “Maternal Mortality: Why Rural Pakistan Needs Better Midwifery Services.”